Reducing the risk of heat illness
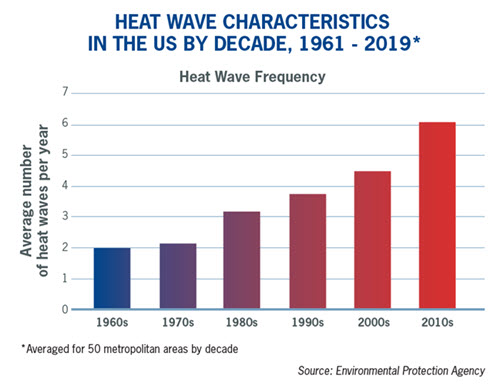
We hear it in the news every day: As the Earth’s climate has warmed, hotter-than-usual days and nights are becoming more common all over the world. April 2022 was the third-hottest month that India has seen over the past 122 years, according to government officials. Closer to home, heat waves are occurring more often in major cities across the US. Their frequency has increased steadily, from an average of two heat waves per year during the 1960s to six per
year during the 2010s (Environmental Protection Agency).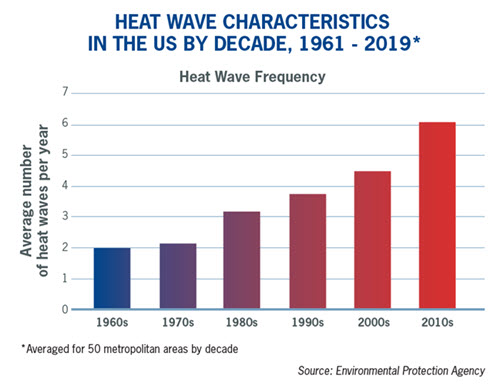
As one might expect, increases in heat waves can lead to heat-related illnesses and deaths in the workplace. Environmental conditions such as air temperature, humidity and sunlight certainly play a role in heat-related fatalities (43 work-related deaths in 2019, per the Bureau of Labor Statistics). However, employers should also consider other factors when identifying hazardous heat exposures for employees who work both inside and outside. These include:
- Heat sources such as ovens, furnaces, and other heated processes
- Level of physical activity leading to body heat production
- Clothing or protective gear that may affect the body’s ability to eliminate heat
- Individual “risk factors” such as employee health conditions (e.g., diabetes, heart or respiratory disease, high blood pressure, etc.), use of alcohol/drugs, medications or varying levels of fitness
Heat Stress and Occupational Exposures
Heat stress occurs when the body cannot eliminate excess heat due to working in a heated environment, wearing restrictive clothing or due to other individual risk factors previously noted. Heat stress causes the body’s core temperature to rise and heart rate to increase. Heat stress can cause symptoms including confusion, dizziness, fatigue, cramps, and nausea, and could lead to illnesses such as heat exhaustion or heat stroke.
Experts believe that heat stress can cause numerous occupational injuries like falls, struck-by incidents, machinery accidents, and vehicle accidents. Heat stress may also contribute to near misses due to employee fatigue or distraction.
Examples of industries with potential heat stress exposures include landscaping services, solid waste collection, sheet metal manufacturing, commercial bakeries, building or road construction, motor vehicle parts manufacturing, police/fire/EMS, and public entities/townships who offer swimming pools (e.g., lifeguarding) and park services.
Recognizing Heat Hazards
Recommendations for Employers
Hazard identification includes recognizing heat hazards and the risk of heat illness due to high temperature, humidity, sun and other thermal exposures, work demands, clothing or personal protective equipment, and personal risk factors. Below are recommendations for reducing the risk of work-related heat hazards.
Use Heat Stress Tools to Identify Hazards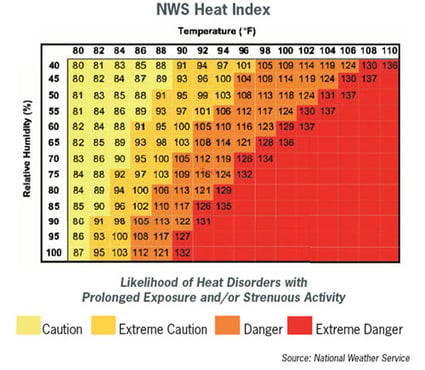
One way to identify heat stressors is by using the following tools:
OSHA’s Heat Safety App: This phone app uses a “feels like” measure of how hot it feels when relative humidity is considered with the actual air temperature. It also offers first aid suggestions for different types of heat stress.
Heat Stress Monitor: These devices measure heat stress in direct sunlight and take into account temperature, humidity, wind speed, sun and cloud cover.
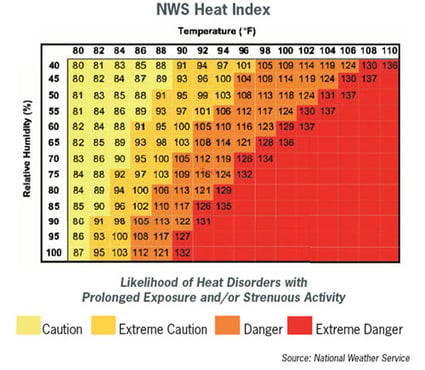
National Weather Service Heat Index: This chart measures how hot it really feels when the effects of humidity are added to high temperatures.
Other Recommendations
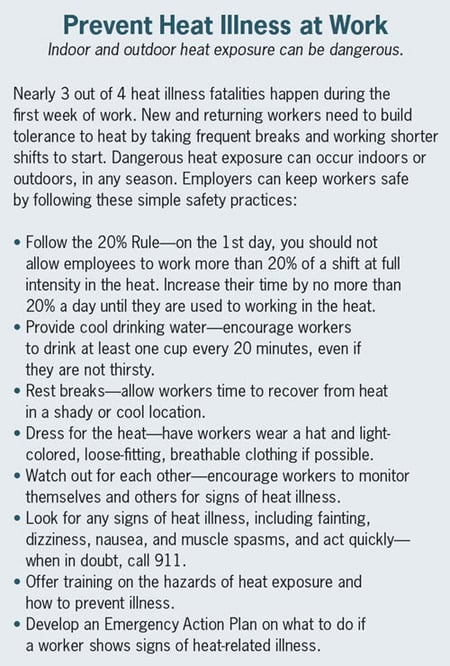
Acclimate Workers: Adapt workers to their environment by exposing them for progressively longer periods to hot work environments. New workers and those returning from a prolonged absence should gradually begin working in the heat. Schedule work during cooler hours of the day. Provide cool water or liquids to workers and have them avoid drinks with caffeine, alcohol or large amounts of sugar. Provide shaded rest periods or an air-conditioned room with water breaks. Use air misters and air-cooled garments.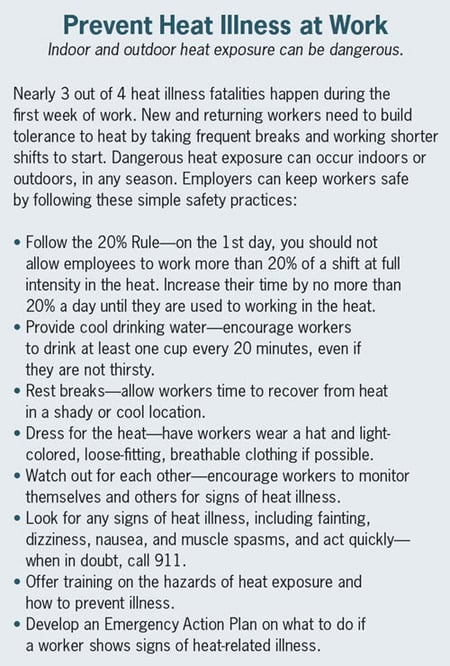
Monitor At-Risk Workers: Supervisors should monitor workers who are at risk of heat stress. Workers who are 65 years of age or older, are overweight, have heart disease or high blood pressure, or take medications may be affected by extreme heat. Use a buddy system and avoid having employees work solo — especially in areas of high heat. Look out for heat-induced illness signs such as being confused or loss of consciousness.
Offer Training: Provide heat-stress training that includes information about worker risk, prevention, symptoms, and the importance of monitoring oneself and coworkers for symptoms.
Create an Emergency Plan: Have an emergency plan and communicate it to supervisors and workers. Emergency plan considerations include:
- What to do when someone is showing signs of heat illness
- How to contact emergency help
- How long it will take for emergency help to arrive; and how to train workers on appropriate first aid measures until help arrives. OSHA’s heat safety app identifies the signs and symptoms of heat stroke, along with first aid suggestions, including moving the employee to a shaded area, removing outer clothing, cooling quickly with water or an ice bath if possible, or calling 911 if medical care is not available.
If you have any questions or would like additional information, please contact your local PMA Risk Control Consultant or reach out to us at heretohelp@pmagroup.com.
IMPORTANT NOTICE
The information and suggestions presented by PMA Companies in this risk control technical bulletin are for your consideration in your loss prevention efforts. They are not intended to be complete or definitive in identifying all hazards associated with your business, preventing workplace accidents, or complying with any safety related or other laws or regulations. You are encouraged to alter the information and suggestions to fit the specific hazards of your business and to have your legal counsel review all of your plans and company policies. PMA Companies and Old Republic Companies do not provide legal advice and the information and suggestions in this bulletin should not be considered as such.